Recently, there was this news that a high school student's eye vision suddenly decreased significantly. He went to the local eye clinic and was thought to only need to replace a new pair of prescription eyeglasses and a series of tests to do down. The diagnosis shows that not simply eye prescription deepening but suffering from Keratoconus needs further treatment.
For most people, Keratoconus sounds unfamiliar, but its incidence is actually not low. If left untreated, it may cause a range of vision disorders, such as vision loss, blurred vision, and corneal edema.
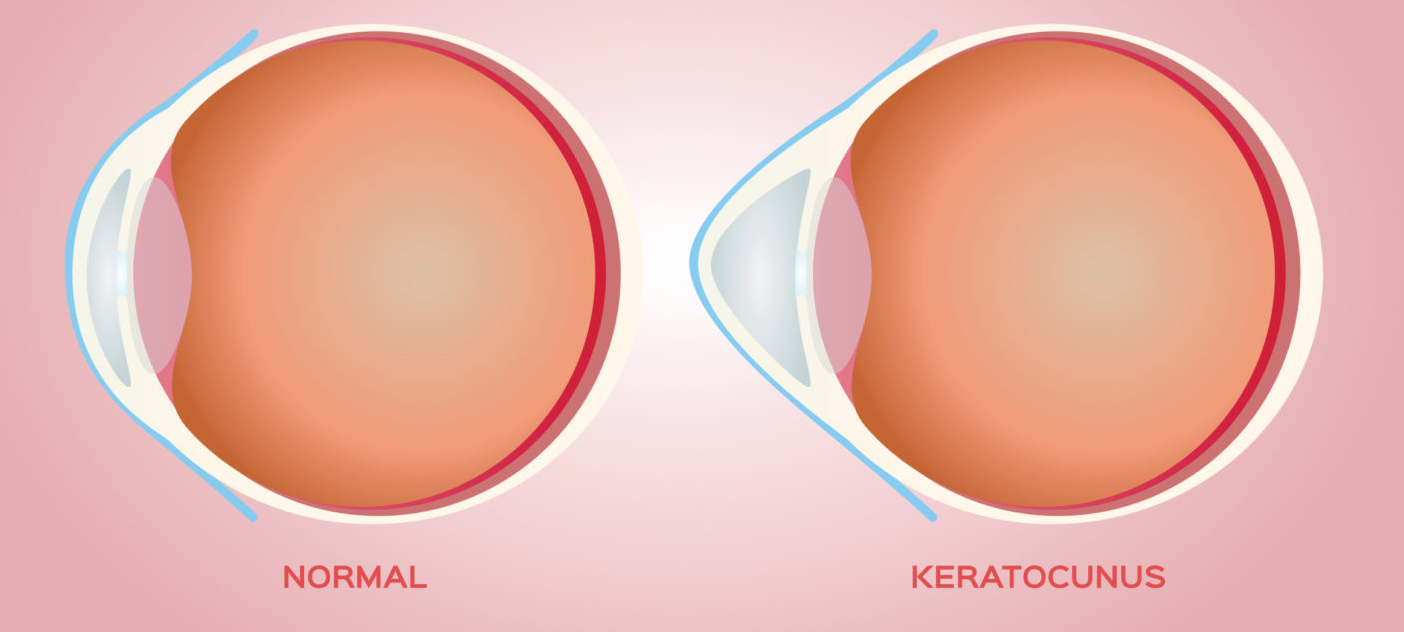
Keratoconus is a corneal lesion in which the cornea is dilated, thins in the center, and bulges forward in a "conical" shape. It usually causes vision loss and irregular astigmatism, and if left untreated, it can eventually lead to corneal perforation and even blindness.
Keratoconus tends to occur in teenagers, with adolescents and young adults between the ages of 15 and 35 being the main groups affected. They usually manifest as a rapid increase in myopia and astigmatism, with no other apparent symptoms, so at first, many people think it is simply a deepening of myopia and does not realize that it is the Keratoconus that is causing the vision loss.
Later, as the condition further develops, myopia or astigmatism worsens and gradually cannot be corrected with prescription glasses, and by the time it is discovered, it has often caused irreversible damage to the vision. It is only then that the seriousness of the problem is realized. Therefore, Keratoconus is also known as the "invisible killer" of youth vision.
In the early stages of cone keratoconus, myopia and astigmatism may appear in one or both eyes, with a progressive increase in myopia and astigmatism in one or both eyes, often with high and irregular astigmatism. Therefore, people with these symptoms should seek medical attention promptly, especially if they have unsatisfactory vision correction with prescription glasses, a history of eye allergy and long-term eye rubbing, or a history of corneal refractive surgery; they should be alert to the possibility of keratoconus.
The pathogenesis of Keratoconus may be related to genetics and environment. Clinical observations have revealed that environmental factors such as prolonged and vigorous eye rubbing, eye pressure caused by sleeping posture, and other mechanical elements may be involved in developing Keratoconus.
Therefore, we should not rub our eyes frequently in daily life, and early intervention and correction of bad sleeping posture. For example, many people like to take a nap on the table with a hand instead of a pillow during lunch break; in the long run, the eye and cornea can easily change shape under the action of external forces and become a Keratoconus, especially the youth cornea is soft, ductile, affected by bad habits, the possibility of higher incidence. Therefore, parents should pay attention to early screening, as far as possible, to detect the early "seeds" of Keratoconus and timely intervention to avoid the progress of the disease to the stage of surgery.